The Right Fit
By Alisa Zapp Machalek
UF pharmacy Professor Julie Johnson is using genetics to fine-tune prescriptions
The blood thinner warfarin is one of the world’s most widely prescribed drugs, but it was originally marketed — and is still commonly used — as a rat poison.
The Renaissance scientist Paracelsus is credited with saying “the dose makes the poison,” and in the case of warfarin and many other common medications, the dose can be the difference between killer and cure. But a safe dose for one person might be dangerous — even lethal — for another.
So how do doctors know how much of a medicine to prescribe? Essentially, they make an educated guess based on all the available information about the patient and the drug. Then they carefully monitor the patient’s response and adjust the dose accordingly.
Unfortunately, for very sick patients — or for very strong drugs — the delay caused by this trial-and-error process can be harmful or even life-threatening.
Julie Johnson, a clinical pharmacist at the University of Florida, hopes to speed things up, getting the right prescription to each patient faster. To do this, she focuses on genes.
“The hope is that through a person’s genetics, we can minimize the trial-and-error process and quickly identify the drug therapy that will work best for that person,” Johnson says.
The ultimate goal is to enable doctors to tailor prescriptions for each patient.
This area of research is called pharmacogenetics or pharmacogenomics. Johnson’s team is one of 14 groups that are part of the Pharmacogenomics Research Network, a nationwide group of scientists funded by the National Institutes of Health.
In addition to determining whether you will be tall or short, black-haired or blond, your genes influence how your body responds to medicines.
But genes aren’t the only factor. Your age, weight, lifestyle and other characteristics may also play a role.
Working Out Warfarin
Warfarin, the rat-poison-turned-blood-thinner drug, is a perfect example of how genes affect the way different people respond.
Every year, an estimated 2 million Americans start taking warfarin, mostly to prevent blood clots that could cause a stroke or heart attack.
Warfarin is a touchy drug. If the dose is too high, a person could bleed to death. If it is too low, a potentially fatal blood clot could form.
And here’s the kicker: the ideal dose varies widely — one person may require 10 to 20 times more than another — so it’s nigh impossible to get every prescription right the first time.
How do doctors even know where to start?
Typically, they begin with the average dose in the population, usually 5 milligrams per day. Then they wait up to a week, check the patient’s blood for its clotting ability, and tweak the dosage as needed.
They repeat these steps for a few weeks (or sometimes months) until they’ve found the optimum dosage. The patient then remains on the final, stable dosage (with regular tests to check that it’s still the right fit).
Doctors have been doing this for decades and have carefully worked out the technique, but Johnson and her colleagues think there’s a better way through pharmacogenetics.
Johnson discussed this idea with other scientists from the pharmacogenetics research network and from the online knowledge base PharmGKB. They all knew that to fully investigate whether pharmacogenetics could improve warfarin dosing, they would need a worldwide effort.
So they created the International Warfarin Pharmacogenetics Consortium, made up of about a hundred researchers on four continents.
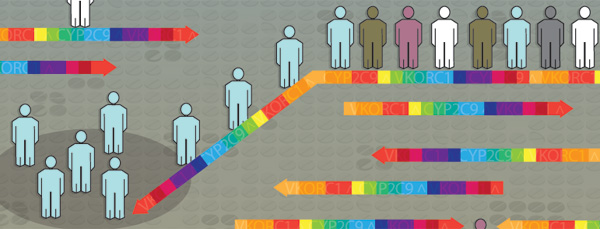
The scientists already knew that variations in two genes, CYP2C9 (an enzyme that breaks down or metabolizes warfarin to make it inactive) and VKORC1 (an enzyme that activates vitamin K), could influence warfarin’s effectiveness. But no one was really sure whether knowledge of a patient’s CYP2C9 and VKORC1 variations could help doctors arrive at the optimal dose of warfarin more quickly. That’s what the consortium set out to determine.
To make the broadest discoveries in pharmacogenetics, scientists have to include patients from around the globe.
By combining their data, consortium members had access to information from about 5,700 patients on stable dosages of warfarin. The patients came from around the globe: Taiwan, Japan, Korea, Singapore, Sweden, Israel, Brazil, Britain and the United States.
This kind of study — one that includes people of different races, ethnicities and lifestyles — is essential to drawing conclusions that are applicable to a wide range of people.
From this vast pool of data, the consortium members created a computer program to predict the ideal warfarin dosage for each patient based on his or her genetic variations and clinical information like age and body size.
Then the scientists checked their predictions against the actual dosage for each patient. (These stable dosages had been established the traditional way — they were initially based on standard clinical factors, then adjusted until they were optimal.)
The genetically based computational predictions were closer to the stable dosages than were the starting dosages obtained using the standard, best-guess method.
The computer program performed especially well for patients at the low or high ends of the dosing range. This got the scientists’ attention, because nearly half of the people on warfarin are at the extremes of the range, and they are the ones most susceptible to dangerous bleeding or clotting.
“In this study, we used data from the largest, most diverse group of patients to date to develop a method for using genetic information in combination with other patient information to determine the dosage of a very commonly used drug,” Johnson says. “This is one of the top five drugs that cause hospitalizations for adverse effects. The real value will be to patients getting warfarin therapy prescribed for the first time.”
The consortium published its findings in the New England Journal of Medicine. Now the strategy is being tested in a large clinical trial to determine whether a gene-based approach to prescribing warfarin will improve the effectiveness and safety of the drug for new patients. The trial is called Clarification of Optimal Anticoagulation through Genetics (COAG), and Johnson is leading a clinical site at the University of Florida.
Pressure Point
Johnson has also focused on drugs that treat high blood pressure, or hypertension, a condition that affects about a third of all adults in the United States.
In the case of warfarin, genes influence how much of the drug a patient needs. For drugs that treat hypertension, genes influence which drug — there are dozens — would be best for each patient.
“There are five first-line drug classes, with probably an average of seven to eight drugs in each class, then an additional half-dozen or so other drug classes that aren’t considered first-line,” Johnson said. “This means there are many choices for drug therapy in hypertension — a good thing — but that also adds to the trial-and-error element of finding the right drug for the right person. If doctors randomly pick one of those medicines, there’s only a 50-percent chance that it will work.
“We’re trying to find out if there are genetic markers to use to pick the right medication from the outset,” she continues. “Right now, it’s a trial-and-error process. It can be very frustrating for patients, especially for young people who aren’t used to taking medicine every day.”
Too often, people get fed up when doctors repeatedly change their medications, she says. The patients feel fine — hypertension has no obvious symptoms — and they may not understand the importance of finding an effective medicine that controls their blood pressure.
“So they go untreated for an extended period. And that’s bad; their chance for heart attack, stroke, heart failure and kidney failure goes way up with extended periods of uncontrolled blood pressure” Johnson says.
Even though they can’t feel it, the extra force of blood pressing against artery walls can seriously damage internal organs. Long-term consequences include kidney failure, strokes, heart attacks, heart failure and death. Because of this, hypertension is sometimes called the “silent killer.”
The condition is hard to study because it is influenced by many factors, including genetics, diet and exercise.
“Hypertension isn’t just one disease,” Johnson says. “It’s reflected in one way — high blood pressure — but it’s really a half dozen pathophysiologies at least.”
The underlying cause — or pathophysiology, as Johnson puts it — of each person’s hypertension points to the best way to lower that person’s blood pressure.
One type of drug for hypertension (beta blocker) works by blocking nerve signals that make the heart beat faster and harder. Another type (diuretic) increases urination and relaxes blood vessels. A third (calcium channel blocker) relaxes heart and blood vessel muscles by keeping out the calcium ions these muscles need in order to contract.
“There’s probably a right medicine out there for every patient, but finding that is the trick,” she says.
Since 2005, Johnson’s lab has received more than $20 million from the National Institutes of Health to study the genetics of hypertension medications, including a five-year, $10.6 million grant awarded in September 2010.
Johnson’s research team has identified a number of gene variations, or genotypes, that influence how people respond to blood pressure-lowering drugs. They have also found genotypes associated with dangerous, long-term complications from hypertension.
“In one study, carriers of a particular genetic variation had an approximately 43 percent higher risk of death, heart attack or stroke,” she says, adding that this type of research “helps us piece together the puzzle of the various genes that lead to some people having worse outcomes than others when they have hypertension.”
And, conversely, which drugs work best for people with these genotypes.
Ultimately, Johnson says “the long-term goal is to guide the selection of medication for an individual patient. In that scenario, physicians would order a genetic test and based on it they would narrow down the drug possibilities that would be best for that individual patient.”
Doctors would be able to look up a patient’s genotype to find the right medicine and/or dose for that person — or at least find out what not to prescribe.
“We’re not quite there yet,” she says. “But we think we’re getting close.”
Maybe then, we’ll be able to modify Paracelsus’ words from “Only the dosage distinguishes the killer from the cure,” to “Now genetics help us distinguish the killer from the cure.”
A version of this article originally appeared in Findings, a publication of the National Institute of General Medical Sciences.