|
downloadable
pdf
Whether
it’s the bite of the dentist’s drill, the viselike
contractions of childbirth or the crushing pressure of a heart
attack, one thing’s certain: Pain is commonly feared
yet poorly understood.
The sensation may be universal, but the intensity with which
it is felt varies widely, colored by past experience, anxiety,
insomnia, cultural conditioning and fundamental biological
or psychological makeup. Now research at the University of
Florida is adding credence to the realization that factors
such as age, gender, ethnicity and even our genetic wiring
play an important role in pain perception.
 |
In
a flash, the damage activates a network of nerves, which
send a warning signal to other nerves in the spinal cord
that then transmit the information to the thalamus in
the brain. From there, the alarm spreads to other brain
regions. But everywhere along that pathway, changes can
occur to alter the experience of pain. |
No fewer than 50 UF scientists are involved in a campuswide
boom in pain research. They are involved in more than 78 diverse
research projects, many through three thriving pain centers
based at the Health Science Center that account for at least
$12 million in federal grant money.
“There’s just an enormous amount of research going
on, everything from bench science with animal models and tissues
to human outcome studies,” says UF psychologist Michael
E. Robinson, who directs UF’s Center for Pain Research
and Behavioral Health, part of the College of Public Health
and Health Professions. “We are really rapidly becoming
one of the biggest universities in the nation to look at pain.”
Experts say properly assessing and treating pain is a huge
challenge. The National Institute of Neurological Disorders
and Stroke reports that chronic pain afflicts nearly 90 million
Americans. Pain is the number one reason patients visit physicians,
and the second most-common reason to miss work, next to the
common cold, Robinson says.
“It could certainly be argued that pain is the most
prevalent and most expensive public health problem in the
United States today,” says Roger Fillingim, an associate
professor at UF’s College of Dentistry who teaches a
graduate-level course on the neurobiology of pain. “It
is estimated that more than 20 percent of the population is
experiencing chronic pain at any given time.”
The price tag is hefty: Medical bills, lost income and productivity,
workers’ compensation and legal expenses associated
with chronic pain are estimated at well over $100 billion
a year — more than is spent on cancer and cardiac disease
combined.
The interest comes at a critical time. Congress has mandated
the first 10 years of this century the Decade of Pain Control
and Research. And the agency that accredits U.S. hospitals
— the Joint Commission on Accreditation of Health Care
Organizations — now requires caregivers to monitor and
document pain as a fifth vital sign, along with blood pressure,
pulse, respiration and temperature.
Lured by the diversity of pain research at UF, Bob Yezierski
left the University of Miami a little over two years ago to
direct UF’s newly established Comprehensive Center for
Pain Research, a cooperative effort of the McKnight Brain
Institute and the College of Dentistry. One of the center’s
goals is the development of clinical and basic science programs
in pain research throughout the Health Science Center. Yezierkski’s
specialty is the study of pain after spinal cord injury, but
he also is seeking to bolster existing research programs in
aging and neuropathic pain, cancer pain, musculoskeletal pain,
visceral pain and orofacial pain.
“There’s an interesting quote, ‘Pain is
a sensation that everybody needs but nobody wants,’”
Yezierski says. “Pain can play a very protective role
in one’s life. But in a chronic state, pain really serves
no useful or biological purpose. It can severely compromise
quality of life, and it can affect not only the individual
who has pain; it can cascade throughout the family or work
environment by negatively influencing those around the person
with chronic pain.”
In Florida alone, a study conducted through the Florida Pain
Initiative showed that pain is epidemic, and Floridians suffer
more from chronic or recurrent pain than the national average.
Pain Paths
So
what triggers pain? Picture an injury like a burn or a broken
bone. In a flash, the damage activates a network of nerves,
which send a warning signal to other nerves in the spinal
cord that then transmit the information to the thalamus in
the brain. From there, the alarm spreads to other brain regions.
But everywhere along that pathway, changes can occur to alter
the experience of pain, and pain responses among individuals
vary tremendously.
 |
| Fillingim
and his colleagues recently examined sex differences in
responses to pain-relieving medicines and discovered a
potent painkiller appears to work better in women who
carry a gene associated with red hair and fair skin. |
“It will take a lot of research to learn why some people
say ‘Ow’ at one level of stimulation, yet it takes
a completely different level of stimulation to make another
person say ‘Ow,’” says Robinson.
Scientists have been striving for years to understand what
causes many chronic pain conditions. They’ve learned
a great deal about the anatomy, physiology and molecular biology
of the pain system. Fillingim says his work is driven by a
“biopsychosocial” model of pain, which holds that
the experience of pain is sculpted by complex interactions
among biological, psychological and sociocultural factors.
These include mood, expectations, past pain history, age,
gender and ethnicity.
“There has been increased interest in understanding
all these factors so we can assess pain more accurately and
treat pain more effectively,” he says.
UF researchers concede that teasing apart the underlying contributions
of biology and society is no small task.
Women with chronic pain report slightly higher levels of pain
than their male counterparts, for example, but the difference
may be as much the result of how society teaches men to handle
discomfort as it is a consequence of biology.
“Clearly men and women are different in terms of how
we raise them,” Robinson says. “We don’t
understand how much of that is driven by social norms and
how much of that is also driven by biology. There are huge
social influences on men and women’s behavior. There
are these stereotypes about how you should present yourself
in public, and that includes the expression and admission
of pain and seeking care for pain. Why should pain be any
different?”
Studies have shown that when men and women report to clinics
for pain control, men are far more likely to get higher doses
of painkillers and women are more likely to get antianxiety
drugs. Other gender stereotypes abound: Some people presume
women are less tolerant of pain than men. In Western societies,
the masculine role often demands that men maintain a “stiff
upper lip,” stoic in the face of pain. Men, therefore,
may be less willing to report pain when they feel it.
The rationale for studying gender differences in pain,
Fillingim says, is that many of the most common chronic pain
conditions are more prevalent among women than among men.
Indeed, research suggests the burden of pain throughout life
is greater for women than it is for men. Sex hormones such
as estrogen may affect pain sensitivity, but most believe
many factors interact to affect pain perception.
“Your stereotypes may be partly formed by differences
in pain processing, but it’s clear your pain processing
can be altered by your belief systems and your expectations
and your stereotyped behavior,” Robinson says. “It’s
possible we’re not treating people optimally because
we’re not recognizing the sex differences we should,
and we’re inappropriately recognizing sex differences
that we shouldn’t.”
Robinson and colleagues are beginning to evaluate how physicians,
dentists, nurses and other health-care providers are influenced
by such stereotypes. In one study, health practitioners will
review various scenarios that feature male and female patients
of various ethnicities experiencing the same degree of pain.
Each provider then must decide whether to give each person
pain-relieving medications. From the responses, researchers
will determine how gender or ethnicity influenced their decisions.
Mean
Gene
And then there’s genetics. Researchers now know pain
isn’t just a symptom — it may have a genetic component.
“Now people are thinking more of pain as a disease,”
Yezierski says. “They’re starting to consider
that some people can potentially be predisposed to chronic
pain conditions, just as some are predisposed to cancer.”
Meanwhile, findings lend credence to the idea that scientists
could someday maximize the effectiveness of prescription medicines
for patients on the basis of specific genes. Fillingim and
his colleagues recently examined sex differences in responses
to pain-relieving medicines and discovered a potent painkiller
appears to work better in women who carry a gene associated
with red hair and fair skin.
“The ultimate goal would be to do a blood test on somebody,
look at their genetic makeup as well as other chemical, biological
and physical characteristics, plug all that information into
a computer, and the computer would print out a sheet that
says, ‘Okay, this drug, at this dose, is going to provide
this patient the best relief from pain,’” Fillingim
says.
Scientists also are considering whether ethnicity affects
pain perception. In the health-care arena, discrepancies in
pain perception or cultural attitudes about discomfort take
on added import because they may influence whether someone
seeks prompt medical attention. For example, physicians have
long known that blacks wait longer to leave for the hospital
when they have chest pain that might indicate a heart attack.
During the next five years, Fillingim’s research team
will study more than 300 blacks, Hispanics and non-Hispanic
whites to gauge their responses to pain in a laboratory setting.
They’ll also look for differences in levels of one of
the body’s natural painkillers and a key stress hormone
produced in response to pain, and study whether genes may
play a role in the amount of pain reported.
“Given the increasing diversity of our population and
the extremely high prevalence of chronic pain … if we
make the mistake of assuming that the pain experience is identical
across all ethnicities and cultures, then we’re going
to do our patients a disservice,” Fillingim says.
Although the past two decades have witnessed tremendous advances
in the understanding of the neurobiology of pain, the development
of new pain-relieving treatments has been disappointing, Fillingim
says. Two thirds of cancer patients, for example, have poorly
treated pain.
“I think if we’re going to do better in the next
15 to 20 years, we’re going to have to take a different
approach,” he says.
A better understanding of the molecular biology of pain could
someday lead to gene therapy for pain management, Yezierski
says. And UF researchers are considering research projects
aimed at identifying biomarkers for pain diagnosis and management.
For now, the most effective management strategy for chronic
pain is a multidisciplinary approach that takes advantage
not only of pharmacology or drugs but also psychological counseling,
group therapy, physical and massage therapy, and exercise,
Yezierski says.
“A lot of different factors contribute to the pain experience,”
he says. “It’s been demonstrated repeatedly that
attacking pain from all these different dimensions usually
leads to the most successful outcome.”
Roger B. Fillingim
Associate Professor, Division of Public Health Services and
Research, College of Dentistry
(352) 392-4539
rfillingim@dental.ufl.edu
John R. Graham-Pole
Professor, Department of Pediatrics, College of Medicine
(352) 392-5633
grahajr@peds.ufl.edu
Michael E. Robinson
Professor, Department of Clinical and Health Psychology,
College of Public Health and Health Professions
(352) 273-6617
merobin@ufl.edu
Robert
Yezierski
Professor, Departments of Orthodontics and Neuroscience,
College of Dentistry
(352) 392-4081
ryezierski@dental.ufl.edu
Related
Web sites:
http://www.painlab.org
http://painresearch.ufl.edu
http://www.med.ufl.edu/rheum
HeArts
& Hope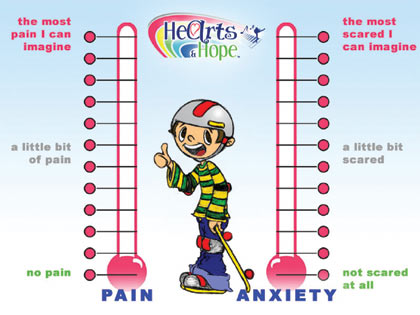
Jay
Klein avoided the Vietnam War, but not by choice.
It was the winter of 1973, and, having pulled a not-so-lucky
number seven in the draft lottery, the 19-year-old college
student figured he was on his way. Yet when he reported
for a routine physical exam at the New Cumberland Army
Depot in Harrisburg, Pa., doctors didn’t send
him overseas like he expected. They ordered him to a
urologist instead.
Forty-eight hours later he found himself on a different
sort of front line altogether — battling testicular
cancer in an era when few teens diagnosed with a malignancy
of any kind survived.
After two surgeries and 18 months of chemotherapy, Klein
suffered all the fears and uncertainty associated with
treatment and survivorship in the 1970s. Three decades
later, Klein is cancer-free, keenly aware of what cancer
patients experience and committed to easing their pain,
both psychological and physical.
As executive director of the HeArts & Hope Project,
an innovative University of Florida program that will
use streaming video-on-demand technology to deliver
the arts to children hospitalized with cancer or sickle
cell disease, Klein is helping lead a federally funded
study designed to test whether the distraction of an
“immersive multimedia environment” —
videos on demand coupled with music in surround sound
— can help alleviate pain and anxiety.
“I had procedures. I had a lot of uncertainty
concerning my life and death, concerning pain,”
Klein says. “But I have not seen anything like
these children see today.”
Because their treatment is much more intense, their
short-term physical pain and suffering is probably greater
— and that may well translate into a harder long-term
emotional recovery, he says.
The HeArts & Hope program began when Klein met UF
pediatrician John Graham-Pole and Jill Sonke, director
of the Center for the Arts in Healthcare, at a Tampa
conference. Klein, a musician and the former program
director for the Tampa Bay Performing Arts Center’s
educational initiatives, sketched out his vision to
Graham-Pole and Sonke: a virtual reality-like system
that would seek to soothe a child’s anxiety and
discomfort, potentially reducing the need for opiate
medications and even shortening hospital stays. A system
they could scientifically test.
Klein and Graham-Pole pored over the scientific literature
to learn other ways researchers had used physical space
and the arts to distract patients from pain. Some had
studied headphones in the operating room. Others had
devised sophisticated 3-D virtual reality glasses for
young burn patients.
They submitted a grant proposal for their immersive
multimedia environment project and landed more than
half a million dollars from the Department of Commerce.
Matching funds from community partners and the UF Foundation
brought the total to $1.3 million.
The multidisciplinary HeArts and Hope team includes
researchers from the College of Medicine’s Department
of Pediatrics, the College of Fine Arts and the College
of Public Health and Health Professions. They are collaborating
with artists and technology partners from around the
nation to develop a network of streaming video broadcasts
and video-on-demand for more than 200 children and adolescents
treated at Shands Children’s Hospital for cancer
and sickle cell disease over the next three years. The
images will be projected on 21-inch flat-screen monitors
mounted on swing-arms, enabling patients to keep the
equipment as close as they’d like.
“(After a cancer diagnosis) all of a sudden everyone
wants to play violins and harps, and we understand that
relaxation is a good thing, but we also are finding
out from the children what is comforting to them,
and that may break a lot of assumptions in our adult
world,” Klein says. “These kids may very
well want to rock.”
The concept of distraction is the theory behind the
approach, Graham-Pole says.
“There’s a limited number of pain pathways
or nerve fibers from the site of the pain to the brain,”
he says. “If you can distract the person from
these pathways to be aware of something else with their
mind, then they will be less aware or even not aware
of the pain. Music we know works very well; so does
laughter. We know physiologically they both cause you
to release endorphins, essentially the body’s
morphine.”
Jay Klein
Executive Director,
HeArts and Hope Program
(352) 392-7803
kleinj@peds.ufl.ed
|
|