Scents and Sensibility
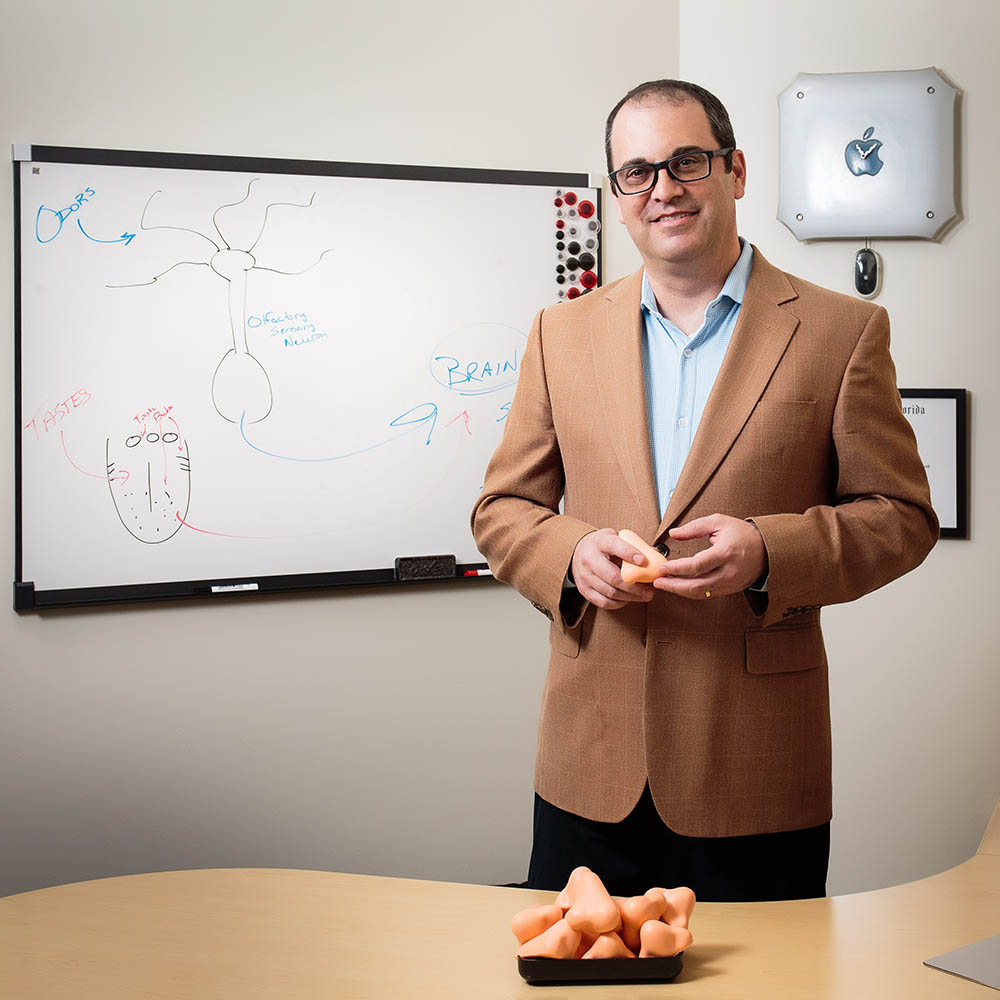
Steven Munger gestures to a bowl of noses.
“Take one,” he offers, catching a visitor staring. “It’s what they’re there for.”
The foam noses bear the logo of the University of Florida Center for Smell and Taste, which Munger directs. With UF Health, the university’s academic health center, the Center for Smell and Taste is launching one of the country’s only clinical programs for people with smell disorders, a problem that sounds insignificant until you’ve lived with it.
About 15 percent of the population has a diminished or distorted sense of smell. More than 16 million Americans live with a smell impairment severe enough to affect their eating habits, their relationships, even their safety. Yet these disorders remain underdiagnosed, little researched, and largely incurable.
With 53 researchers lending expertise to the center, and the UF Health Smell Disorders Program opening January 25, Munger and his colleagues want to change that. But no one knows if people will come to a practice where, for most patients, the only immediate offerings are support and hope.
“There’s not a pepperoni pizza molecule. There’s no rotten fish molecule. How do we take this complex sensory environment and pull it apart so we can deal with it, then put it back together in a way that’s useful?” he said. “That’s a question I will never answer in my lifetime.”
He was happy trying, working on the basic science underpinning those processes. But when he joined the Center for Smell and Taste in 2014, he began to appreciate how widespread smell disorders are and how deeply they impact patients’ lives.
It’s surprisingly easy to lose your sense of smell. Some people are born unable to smell because of a genetic mutation, or from damage to the olfactory nerve during birth. A facial or brain injury later in life can take smell away, as can a viral infection or a degenerative brain disease like Parkinson’s or Alzheimer’s. Some smell loss is age-related, other cases are brought on by environmental toxins, or obstruction or inflammation in the nasal passages. From 1999 to 2009, more than 130 people reported losing their sense of smell after using a widely available homeopathic cold remedy.
The consequences of smell loss can be far-reaching, from safety concerns (what if you can’t tell that food has spoiled, or detect a gas leak?) to practical ones (what if you can’t tell when your toddler has dirty diaper?). A world without smells has social ramifications, too.
“You know you’re missing out on an important aspect of the world that other people are perceiving,” he says. “It can create a sense of isolation.”
Think about never being able to smell your newborn baby, for example, or missing out on the role scents play in memory. Whenever Munger smells lighter fluid, he remembers his grandfather, who quit smoking when Munger was born, but never relinquished his Zippo.
If you lost your sense of smell, you’d also notice a big difference in flavor. To experience how smell affects flavor, hold your nose closed and eat a jelly bean. You’ll still taste sweetness, but you won’t be able to tell if it’s lime or orange. That’s because flavor isn’t just what you taste with your tongue, but what your nose and soft palate contribute. It’s why food doesn’t taste right when you have a cold, and why many people with smell disorders lose the pleasures of eating and drinking along with smell.








